Was dit document nuttig?
Summary Anatomy and Fysiology
Vak: Anatomie en fysiologie (AB_1176)
71 Documenten
Studenten deelden 71 documenten in dit vak
Universiteit: Vrije Universiteit Amsterdam
Was dit document nuttig?

Summary Anatomy and Physiology (AB_1176)
Fundamentals of Anatomy and Physiology; Martini
H20 The Heart
20.1: The heart is a four chambered organ that pumps blood through the systemic and pulmonary circuits
Heart: hollow muscular organ in thoracic cavity – pulmonary (lung, short): carries blood to and from the gas exchange
surfaces of the lungs— and systemic circuit (long, to organs): transports blood to and from the rest of the body
- Arteries carry blood away from the heart, veins return blood—great vessels are connected to the heart; capillaries
(smallest arteries) are interconnected; their thin wall permits the exchange of nutrients, dissolved gasses, and waste.
- Four muscular chambers: (1) right atrium receives blood from systemic circuit and passes it to (2) right ventricle
pumps blood into pulmonary circuit (3) left atrium collects blood hereof and empties into (4) left ventricle pumps
blood into systemic circuit >> first atria contract, then ventricles (equal volumes)
- Great vessels connected to superior end of the heart at its base; third costal cartilage—inferior tip of the heart is the
apex >> heart sits in anterior portion of the mediastinum, between two pleural cavities >> mediastinum contains
great vessels, thymus, esophagus, and trachea
- Walls of heart: endocardium (inner layer), myocardium (spiral bundle of cardiac muscle cells), pericardium (fibrous
and serous membrane) is two layered: parietal and visceral layer which are separated by fluid-filled pericardial
cavity
1. Pericardium >> visceral layer of serous pericardium (epicardium) covers surface of the heart: exposed
mesothelium and underlying layer of areolar connective tissue
>> parietal layer of serous pericardium: outer dense fibrous layer, areolar layer, and an inner mesothelium
2. Myocardium forms atria and ventricles – contains cardiac muscle cells, connective tissue, blood vessels, and
nerves—muscle bundles encircle the great vessels – deeper muscle layers spiral around
3. Endocardium covers inner surfaces of the heart and heart valves – simple squamous epithelium and underlying
areolar tissue
- Cardiac skeleton is supporting (crisscrossing) limits the spread of action potentials: four dense bands of tough
elastic tissue that stabilize positions of heart valves and ventricular muscle
- Pericardium surrounds the heart; pathogens can infect => inflammation => pericarditis (surfaces rub against one
another, making a scratching sound ==> commonly results in increased production of pericardial fluid -> collects in
cavity; restricting movement of the heart => cardiac tamponade (also from traumatic injuries)
> outer fibrous pericardium; dense network of collagen fibers that stabilize position
> inner serous pericardium; outer parietal and inner visceral (epicardium) – potential, fluid-filled space: pericardial
cavity – pericardial fluid secreted by pericardial membranes acts as lubricant -> reducing friction
Two atria have relatively thin muscular walls and are highly expandable – outer portion deflates => lumpy, wrinkled flap:
auricle
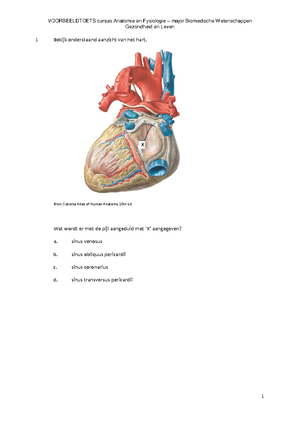
- Coronary sulcus: deep groove, marks border between atria and ventricles: anterior interventricular sulcus and
posterior interventricular sulcus are shallower => boundary between left and right ventricles – fat in sulci
- Connective tissue of the heart includes collagen and elastic fibers (sheath) – fibrous cross-links/ struts interwoven
into sheets (1) provide physical support of for myocardium (2) help distribute forces of contraction (3) add strength
and prevent overexpansion of the heart (4) provide elasticity -> original shape and size
- Chambers are separated by septa – atria are separated by (thicker) interventricular septum – valves: covered
openings >> two atrioventricular (AV) valves: folds of fibrous tissue; extend into openings between (and from: one
direction) atria and ventricles >> two semilunar valves between ventricles and their great vessels
- Right atrium receives blood from superior vena cava (from head, neck, upper limbs, and chest) and inferior vena
cava (from rest of trunk, viscera, and lower limbs) – no valves between venae cavae and right atrium
Formane ovale penetrates interatrial septum and connects two atria of the fetal heart => permits blood flow from right atrium
to left atrium while lungs are developing => closes at birth => sealed
>> fossa ovalis remains at this site in the adult heart
- Posterior walls of right atrium and interatrial septum have smooth surfaces – muscular ridges: pectinate muscles >>
blood travels through flaps: cusps; part of tricuspid valve (right atrioventricular (AV) valve) – free edge of each
cusp attached to chordae tendineae that originate at the papillary muscles
- Internal surface of right ventricle contains series of muscular ridges: trabeculae carneae – moderator band delivers
stimulus for contraction to the papillary muscles => begin tensing the chordae tendineae before the rest of the
ventricle contracts – conus arteriosus ends at pulmonary arteriosus; consists of three semilunar cusps (thick
connective tissue)
- Blood flowing from right ventricle passes through this valve into pulmonary trunk => into left pulmonary arteries
and right pulmonary arteries – vessels branch within lungs before supplying the capillaries